Case Studies
Rehabilitation Audit
Who/Location:
Midwestern U.S. / Level I Trauma Academic Medical Center
What/Needs:
An audit was required for the Inpatient CDI team to be able to determine where opportunities existed. Additionally, it would be determined if standardized query templates would be beneficial for their facility. In conjunction with the inpatient CDI audit, it was found that the affiliated Inpatient Rehabilitation Hospital (IRF) had a CDI staff member as well. Her duties included reviewing acute care inpatient stays and appropriate documentation of the patients in the IRF. The documentation requirements along with code assignment for the IRF are more complex related to the required diagnoses being placed on two separate documents with different requirements. An additional 2 charts from the IRF were audited to determine opportunities and possible vulnerabilities related to documentation.

Processes:
Fifteen inpatient charts per Inpatient were audited. Elements included in the audit process were MS-DRG accuracy, principal diagnosis assignment, and secondary diagnosis codes. When considering queries, missed opportunities and compliance with the submitted queries were reviewed closely. In addition to the inpatient chart reviews, there were 2 IRF charts reviewed. The elements reviewed in the audit of the IRF charts included many elements that are not normally seen in an inpatient review. These elements include determining the best Etiologic diagnosis which is extremely important for payment and compliance with the regulations surrounding an IRF admission. The documentation of the patient’s impairment and the etiologic diagnosis must be clearly linked in the provider’s documentation and it must be done in a certain timeframe. Secondary diagnoses and the sequencing of those codes were also reviewed.
Value Add:
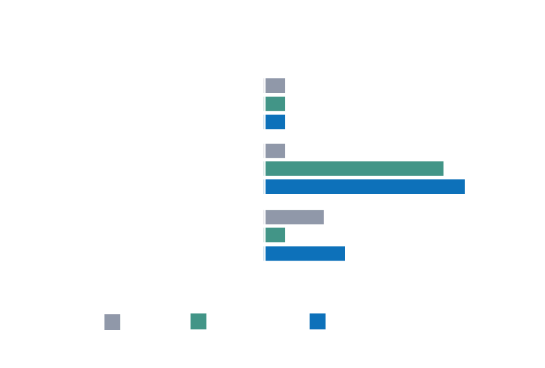
It was found that the overall accuracy score regarding query compliance was in the mid-80s, and that query templates would greatly benefit the facility’s organizations. Medovent staff responded in an advisory capacity by creating query templates, as requested such as: Nutrition Specificity for Malnutrition, and Wound Specificity as it relates to pressure ulcers. Added value to the audits was a customized education presentation that was created, utilizing the opportunities identified in the audit. An additional educational session with accompanying continuing education units, (CEUs) was provided to the facility’s CDI and coding team. Finally, insight was provided on calculating the return on investment for the CDI and coding teams, and for the IRF, as the prospective payment is different as compared to the traditional MS-DRG payment to the acute inpatient facility. Once the action items provided were initiated and put into practice, the facility’s team was able to shrink the loss that was initially discovered. Medovent Solutions is set to conduct another audit on the first of the year.
The financial impact for the initial audit identified a total of $55, 568.44, from query and coding reconciliation opportunities. This resulted in a Case Mix Index (CMI) change of 1.740847 to 2.253567. In addition, a financial opportunity of over 15 thousand dollars was found in one of the 2 rehab cases reviewed.
Inpatient Coding Audit
Who/Location:
Southern U.S. / Level 1 Academic Medical Center (multi-system)
What/Needs:
We offer mid-revenue cycle services such as clinical documentation integrity specialist (CDIS), denial management (DRG downgrading, including clinical validation), and coding (IP and OP facility coding, IP and OP ProFee).

Solution:
We conduct audits and meet their staffing requirements by offering executive summaries and specialized onboarding procedures. This guarantees that the institution selects the best applicant who possesses the knowledge, skills, and professionalism required for success.
Value Add:
We offered a thorough, personalized screening, auditing, and onboarding procedure that gave employees the tools they needed to reduce their DNFB days. It returned much-needed time to the client to finish the numerous things they had on their plate every day, including the 2024 implementation of their new EMR system. This client works with more than nine vendors, and we’ve been informed that we’ve emerged as a genuine partner of choice thanks to our tried-and-true revenue cycle solution procedures. In less than a year, we have placed over 40 consultants and are among the top 2 suppliers used.
Outpatient Audit
Who/Location:
Western U.S. / Level I Academic Medical Center
What/Needs:
The institution, which is part of an ACO/MSSP framework, needed to maintain the coding intensity and severity levels of its patient population, however, they were having trouble with recapture rates for HCCs (Hierarchical Condition Categories). For every Medicare beneficiary, CMS calculates a single HCC risk score in order to forecast costs for the upcoming year. The risk score takes into account both demographic data (such as age, sex, Medicaid dual eligibility, and disability) and diagnostic information from claims data (which is then categorized into HCCs). Because CMS modifies MSSP beneficiary risk scores retroactively, a beneficiary’s 2021 claim data may be the basis for a risk score that determines how much to pay in 2022. Therefore, recapturing HCCs year after year is crucial to an institution’s performance in an ACO/MSSP model; if their risk decreases annually, this might result in a significant financial burden for the institution after year-over-year data analysis and analysis of cost and severity is completed.

Solution:
We created the first OP CDI program for this organization by staffing it with knowledgeable OP CDI specialists, setting KPIs (key performance indicators) that could be monitored to confirm the program’s necessity, collaborating with providers to gain support, and launching a prospective OP CDI query process that was fully operational. To get buy-in for our HCC query process, we engaged with providers and looked at encounters that were paid via the CMS’s traditional fee-for-service system as well as HCC collection. Finally, we developed an OP CDI calculator to continuously assess return on investment.
Value Add:
We eliminated a 69% annual decline in their HCC recapture rate, which also resulted in the admission of over 14,000 patients and the receipt of over $11 million in revenue.
